
LOVE YOUR EXTRAORDINARY CAREER

Registered Nurse Internship Program

Franciscan Travel Program

Patient Care Tech Training Program
Lorem Ipsum
Join the Franciscan Community
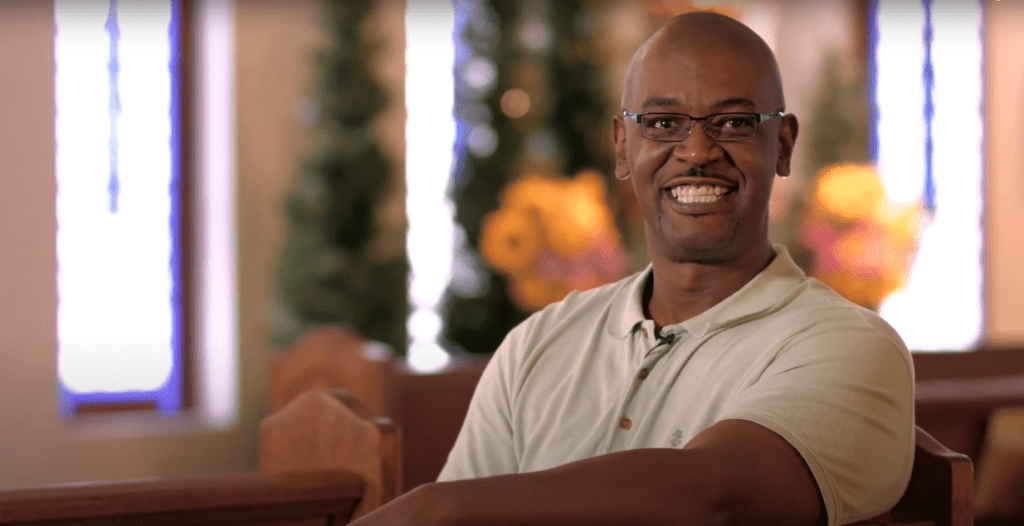
What our employees are saying
What our employees are saying
Loading...

Loading...

Loading...
Learn more about us

OUR BENEFITS
We are dedicated to providing you with access to cost-effective, high-quality benefits.

